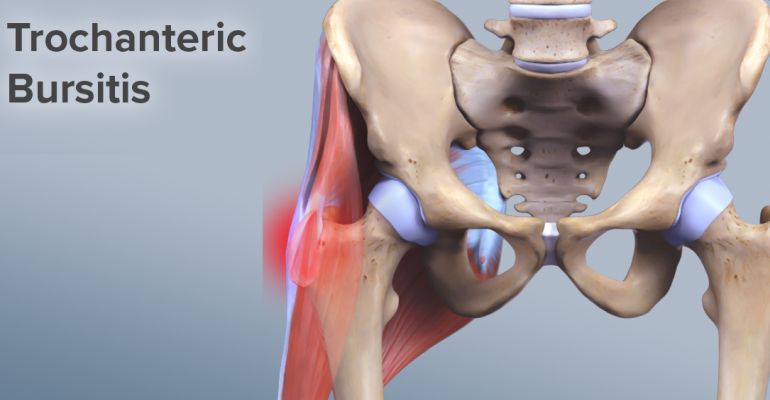
The bursae are small sacs filled with fluid that are found near the joints. The bursae help the joints to move easily, allowing the muscles and tendons to slide over the bones and other structures. The human body has over 150 bursae in its composition.
Trochanteric bursitis occurs when the bursae in the hip become inflamed. Trochanteric bursitis is one of the most common causes of hip pain, explains the orthopaedic in Delhi.
The name of this condition comes from the fact that it affects a bony area called the trochanter. The trochanter is the upper part of the femur and is located at the hip joint.
Signs and Symptoms
Trochanteric bursitis is a common cause of hip pain in active, middle-aged women. This condition can cause significant hip pain, especially if the person is putting pressure on the hip.
People with this condition may also experience the following symptoms:
- Pain that usually occurs on the outside of the hip;
- Pain that worsens during physical activity;
- Pain when climbing stairs;
- Pain when sitting on the affected side;
- Pain on touch and pressure.
The pain associated with trochanteric bursitis is usually more severe at night, especially when a person sleeps on the affected side. If the tendons in the hip are inflamed, the symptoms may be more aggressive.
Trochanteric bursitis may have symptoms similar to those caused by rupture of the gluteus medius muscle, which is a muscle that attaches to the same area.
If symptoms persist and muscle rupture is suspected, an orthopaedic doctor in Delhi should be consulted as soon as possible, as this injury may require surgery.
Causes
Some of the causes associated with trochanteric bursitis include:
Trauma - a history of repeated or severe falls or blows to the hip can cause trochanteric bursitis;
Overuse - people who engage in repetitive physical activities, such as running or cycling, can cause inflammation of the bursae at the hip;
Vicious positions - positions that can put extra pressure on the hips can cause trochanteric bursitis. Posture-related conditions, such as scoliosis, can also cause trochanteric bursitis;
Calcium deposits or bone spurs - sometimes a person can develop additional bone growth on the trochanter. They can rub against the bursae, leading to their irritation and inflammation;
History of chronic diseases - people with chronic diseases, such as gout, thyroid disease, psoriasis and rheumatoid arthritis, may be at increased risk of developing trochanteric bursitis;
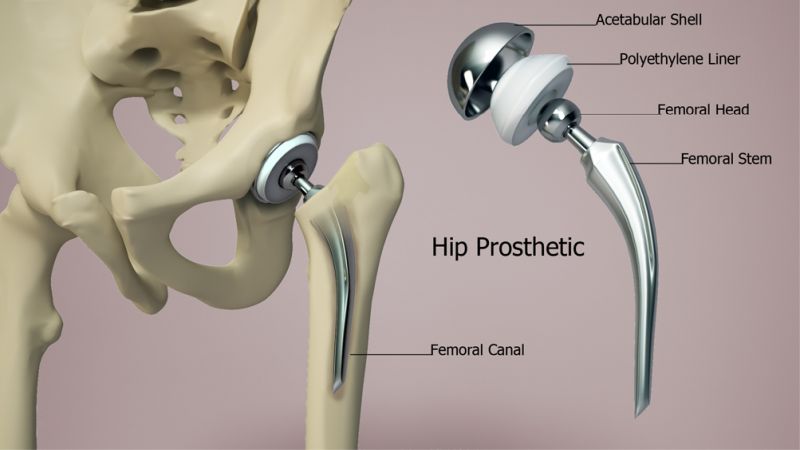
Background Surgery - A person is more likely to develop trochanteric bursitis if he or she has had hip surgery in the past.
Between 3-17% of people with hip prostheses have developed trochanteric bursitis. Sometimes, hip replacement surgery in Delhi can result in a slight difference in leg length, which can also contribute to the appearance of trochanteric bursitis;
Overweight - overweight or obesity are factors that can contribute to the development of trochanteric bursitis. This is due to the fact that being overweight puts more pressure on the hip and the area around it.
Establishing the Diagnosis
The orthopaedic in Dwarka will begin diagnosing trochanteric bursitis by first examining a person's medical history, along with the associated clinical picture.
Also, for diagnosis it is necessary to physically examine the balance, detecting delicate areas near the place where the bursae are located. In some cases, the doctor may feel areas of bulging tissue in the affected hip.
In addition to the physical exam, your orthopaedic in Delhi may recommend additional medical imaging tests to check for abnormalities associated with the condition. These investigations include:
- Radiography;
- Bone density tests;
- Magnetic resonance imaging (MRI).
The orthopaedic doctor in Dwarka will consider not only the symptoms that indicate trochanteric bursitis, but will also try to rule out other similar conditions. These include:
- Osteoarthritis;
- Fibromyalgia;
- Bone fracture in the upper femur;
- Hip dislocation.
Treatment Options
Treatment options used for trochanteric bursitis include:
Rest - to give time to inflamed bursae to heal. Sometimes a person with trochanteric bursitis may need special devices to move, such as crutches. Avoiding activities that have caused trochanteric bursitis is indicated in most cases.
Non-steroidal anti-inflammatory drugs - they help reduce pain and inflammation. Because these drugs can cause side effects, such as stomach pain and bleeding, it is recommended to use them in the short term.
Applying ice - ice can reduce inflammation and help manage pain.
Physical therapy - engaging in various physical exercises recommended by therapists can help improve range of motion and strengthen the muscles around the hip.
The physical therapist may use other treatments, such as massage and ultrasound.
Corticosteroid injection - your orthopaedic in Delhi may recommend these injections to reduce pain and inflammation.
Weight loss - weight loss is indicated for overweight people. Excess weight puts your hips under extra pressure, resulting in severe pain.
If these methods of treatment are not effective, as the patient is still in pain, the doctor may recommend surgery. Surgery is performed by the orthopaedic surgeon in Delhi only if symptoms have not improved after 12 months of medical treatment.
In extreme cases, a person can remove their bursae by minimally invasive techniques. The procedure can be performed laparoscopically, through very small incisions, using a small chamber to guide the surgeon.
Removal surgery does not usually involve hospitalizing the patient, and recovery takes only a few days.
Perspective
Trochanteric bursitis can be a difficult and painful condition. Usually, drug treatments with nonsteroidal anti-inflammatory drugs can help improve the clinical picture. Surgery is the last recommended treatment method for those with persistent painful symptoms, says the orthopaedic in Delhi.
A person is more likely to develop trochanteric bursitis as they get older, and women are at higher risk than men. The outlook is generally favorable, but it depends on how quickly the treatment is installed.