The meniscus is a semi-circular structure inside the knee located between the joint areas of the femur and tibia.
The meniscus distributes the load and protects the articular cartilage, and also partly gives stability to the knee while walking. Inside the knee are two menisci - internal and external. The external meniscus is more mobile; therefore, it is injured much less often. A meniscus injury is a fairly common occurrence, which is most common among physically active citizens.
Despite this, in a small number of cases, menisci are damaged during various degenerative processes inside the knee, for example, osteoarthritis, explains orthopaedic in Delhi.
HOW IS MY KNEE ARRANGED?
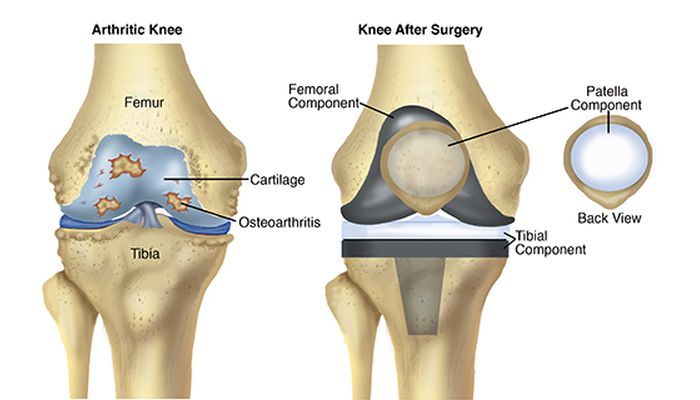
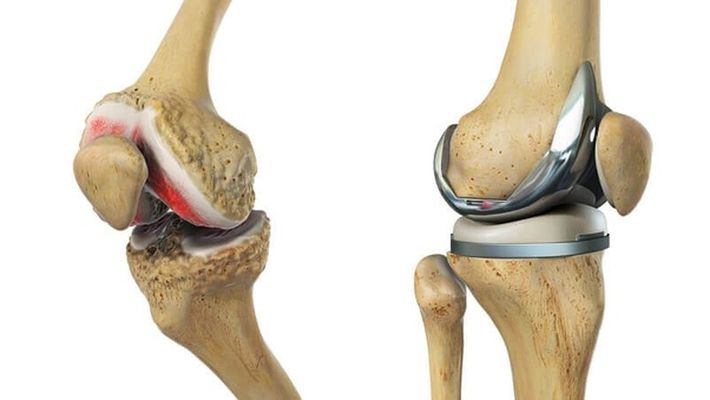
The knee joint consists of three bones (femur, tibia, and patella), connected rigidly together with the help of ligaments that stabilize the joint. The articulating surfaces of the bones inside the joint are lined with a smooth protective tissue called articular cartilage, it allows the bones to glide relative to each other.
With arthritis and arthrosis, as well as damage to the menisci and ligaments, cartilage is significantly damaged.
Ligaments are dense structures of connective tissue that hold bone to bone and stabilize the knee. Inside the knee joint are two main ligaments. An anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). They cross crosswise in the center of the joint, from which they got this name. The other two main ligaments are actually located outside the knee joint, on the outside and inside of the knee. They act to stabilize the lateral movement of the knee.
The ligament on the inside of the knee is called the medial collateral ligament or MCL. The ligament on the outside of the knee is called the lateral collateral ligament or LCL.
The patellar ligament connects the lower pole of the patella with the upper part of the lower leg. The central third of this ligament is sometimes used as a source of graft when restoring a torn anterior cruciate ligament.
The meniscus is a crescent-shaped or C-shaped structure located between the joint areas of the thigh and lower leg. There are two menisci in each knee, one on the inside called the “medial meniscus” and one on the outside called the “lateral meniscus”.
The meniscus is one of the varieties of cartilage. The meniscus can be torn during twisting movements in the knee. Rupture can occur along the inner edge of the meniscus, or, less commonly, along the outer edge. There can also be only a small meniscus gap, for example, a patchwork or a large so-called “handle-watering” gap; it represents a gap along the entire length of the meniscus. Such a gap can block the joint, which means that the leg cannot be straightened to the end. All types of meniscus tears can be successfully treated with arthroscopy in Delhi.
WHAT IS THE MECHANISM OF MENISCUS DAMAGE?
Menisci most often burst during sports, with sharp rotational and rotational-flexion movements in the knee, deep squats, and jumps. A torn meniscus fragment moves into the joint cavity during movements and causes sudden pain and periodic blockages. Meniscus tears are often accompanied by trauma to the cruciate and lateral ligaments of the knee. Due to the peculiarities of meniscus nutrition, they grow to the place of separation extremely rarely, says orthopaedic in West Delhi.
HOW CAN YOU SUSPECT A MENISCUS INJURY?
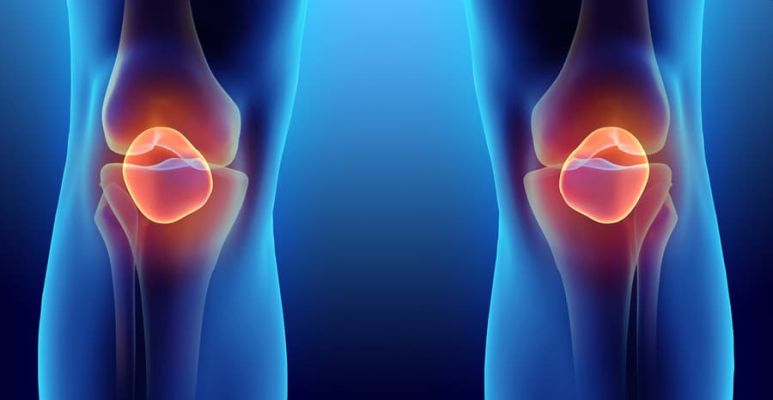
Common symptoms with a fresh joint injury are inflammation, severe pain, limited mobility in the knee, and fluid buildup in the joint. According to the abatement of the acute period, after a few weeks, the symptoms characteristic of the meniscus rupture come to the fore: local pain at the level of the joint space, “clicks”, “crackling” during movements, muscle hypotrophy, inflammation of the synovial membrane with the formation of effusions, periodic blockages.
HOW TO DIAGNOSE MENISCUS INJURY?
The menisci of the structure are cartilaginous; therefore, they are not visualized on x-rays. The diagnosis is made by a specialist orthopaedic in Dwarka based on complaints, clinical test results, and magnetic resonance imaging data.
WHAT TO DO IMMEDIATELY AFTER AN INJURY?
Immediately after a knee injury, orthopedic in Delhi recommends:
- immediate limitation of knee loads, moving on crutches;
- placing a cold compress on the joint, this will reduce pain and swelling, as well as stop bleeding inside the joint. - it is better to use an orthosis or gypsum in a pinch for fixing the knee;
- giving the limb an elevated position will also help reduce swelling and pain in the knee;
- take non-steroidal anti-inflammatory drugs.
HOW TO CURE A TORN MENISCUS?
Treatment of meniscus lesions is more often surgical. Using arthroscopy of the meniscus, partial (partial) or less often complete removal is performed. It is also possible to put stitches on the meniscus and fix it to the tear point, but unfortunately, this does not in all cases give the planned result.
With minor injuries of the meniscus, non-surgical treatment is possible. Indications for surgery are large gaps characterized by mechanical symptoms (clicks, crunching, pinching, limitation of mobility), the recurrent formation of fluid in the joint, as well as in cases of unsuccessful non-surgical treatment. It is worth emphasizing that with meniscus tears orthopaedic surgeon in Delhi does not advise to postpone treatment and put up with poorly tolerated pain in the knee.
A torn meniscus and its fragments can irreversibly destroy articular cartilage, up to its erasure to the bone. In modern conditions, meniscus surgery is performed using arthroscopy. Arthroscopic intervention is performed through two punctures up to 0.7 cm long. An arthroscope is connected to one of the arthroscopes through the camera to the monitor, and instruments for manipulating the joint are inserted through the other.