Total hip replacement (arthroplasty) is a surgical procedure consisting in replacing the hip joint with artificial parts. Most often, it is people whose degenerative disease destroys the hip joint and causes chronic pain.
The World Health Organization (WHO) has said that approximately 28% of people over 60 years of age have osteoarthritis and, of this group, 80% have limitation in their movements of ordinary life. In India, as we continue to age, the possibility of this reality is becoming more and more frequent.
According to the orthopaedic in Delhi, Osteoarthritis of the hip, in musculoskeletal diseases, is perhaps the one that generates the greatest disability; the functionality of the patient decreases due to loss of movement and disabling pain. But let’s review what osteoarthritis really is to understand its treatment.
Articular cartilage is a specialized tissue that covers every joint, allowing mobility and ideal adaptation in these areas to favour arches of motion.
But how is cartilage formed? They are highly specialized cells called chondrocytes, which differ from the embryonic stage and, when located in the joints, have biomechanical properties; They are capable of supporting the necessary loads associated with movement, walking, etc.
These cells produce collagen, which makes it possible to better support the physiological loads of movement and determine the characteristics of structure and differentiation according to the stimulus. These cells accompany us throughout life in our joints.
The downside is that these cells are not capable of reproducing in vitro and if there is injury or local damage they do not regenerate.
There is still no proven drug that can stimulate the reproduction of new chondrocytes that have the same properties as the original cells. When the cartilage erodes, a cartilage with regular characteristics called fibrocartilage is produced, which is not capable of imitating the original functions of the original articular cartilage. If the injury is considerable, it will inevitably end in osteoarthritis, says the orthopaedic surgeon in Delhi.
Osteoarthritis has different origins. It can be presented by a degenerative process, such as collagen diseases and the best known is rheumatoid arthritis; due to mechanical alteration, as is the case of angular or rotational alterations of the extremities, which wear irregularly the articular surface, for example, untreated hip dysplasia in children will surely end in osteoarthritis at some point in life. Osteoarthritis, too, can occur due to intra-articular fracture, which destroys cartilage and ends in post-traumatic osteoarthritis.
Finally, patients who have been apparently healthy, for genetic reasons and individually end up developing osteoarthritis in a primary way.
The treatment of osteoarthritis is aimed at protecting the function of the joint; This implies controlling the patient’s weight, performing activities of daily living that reduce excessive loads on the compromised joints, maintaining an adequate balance of the muscles around the joints, and understanding that the progression of osteoarthritis will possibly end in a greater compromise, explains the orthopaedic doctor in Delhi.
Each case is different and therefore the approach must be individualized.
On the market they offer different drugs that promise to “improve” osteoarthritis; unfortunately, studies show that the vast majority either do not work or barely achieve a feeling of pain control and a placebo effect. But none have succeeded in making the destroyed cartilage regenerate hyaline cartilage. Caution should be exercised with the use of these options, some of which are expensive and do not guarantee substantial changes.
When osteoarthritis has compromised the hip and the pain becomes disabling, the patient should go to the orthopaedist in Delhi, who will assess the age, work activity, sports and family expectations of the patient. Generally, hip replacement in Delhi will be the option, to control pain and regain mobility.
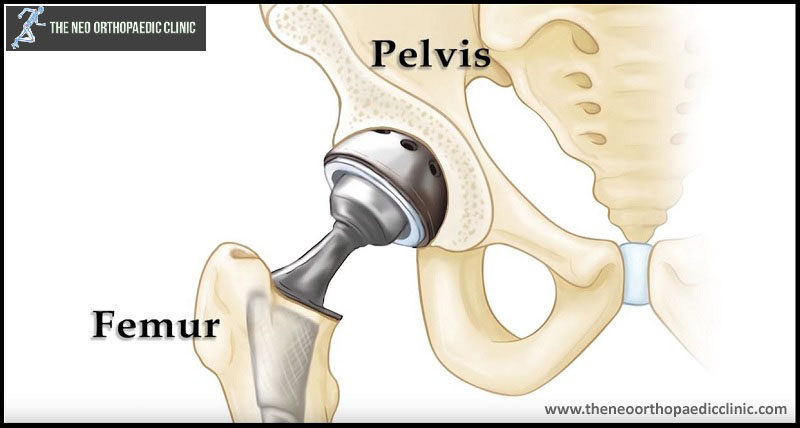
We owe the development of hip prostheses to the British orthopaedist Sir John Charnley, who through experiments on animals and then on humans in the 1940s managed to design and develop hip replacement using bone cement. (methyl methacrylate) to better adapt it to the bone.
This design allowed the hip joint replacement technique to be perfected in the following years, being today one of the most frequent surgeries in the world of orthopaedic surgery.
This managed to change the prognosis of the disease and allowed the patients to have an ordinary life, without pain, and with the functionality necessary according to their condition.
For this reason, when this procedure is defined, one must have the peace of mind of traceability over time, the high performance of prosthetic materials, refined techniques and in-hospital processes that favour a rapid recovery of the patient.
Of course, this hip replacement surgery in Delhi embodies inherent risks such as infection associated with any procedure, thromboembolic disease and other entities that are generally associated with the condition of each patient.
They are risks that are tried to be minimized with guides and protocols that help to give patients an excellent post-operative period and that increasingly show us success stories.
So, when you have hip pain, lameness and functional limitation, go to an orthopaedic doctor in Delhi specialized in traumatology to guide you and improve your style and quality of life.