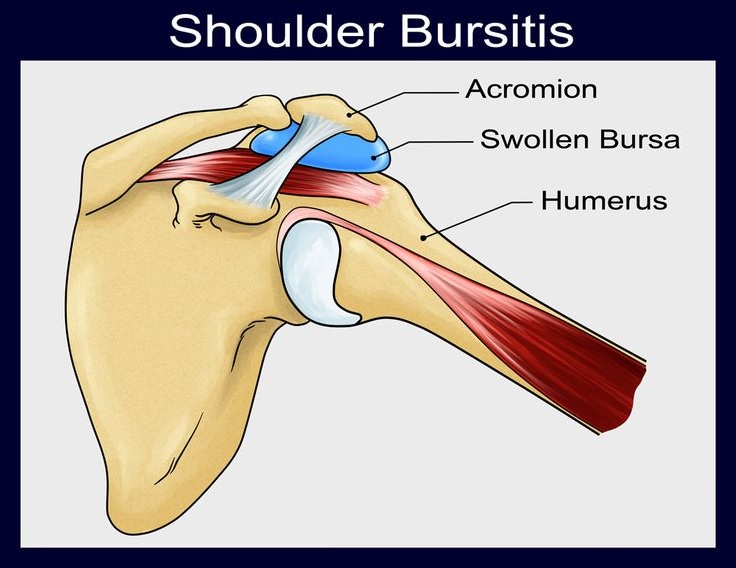
What is shoulder bursitis?
The shoulder bursitis results from an inflammation of the synovial bags (or bursae) that exist around this joint and the tendons of the rotator hood.
It is one of the most frequent causes of pain in this joint. It can be bilateral, reaching both the left shoulder and the right shoulder.
It can be acute or progress to chronic shoulder bursitis, says the orthopaedic in Delhi.
Subacromial bursitis
There are several bursitis that can occur in the shoulder depending on whether one or the other synovial pouch is affected.
The most frequent are those that reach the sub deltoidal subacromial bursa, forming what is commonly called subacromial bursitis.
Shoulder bursitis – symptoms
Shoulder bursitis presents a clinical picture similar to that of tendonitis in the shoulder.
The most characteristic symptoms are the presence of inflammatory pain, located on the antero-lateral face of the shoulder, eventually radiating to the arm and elbow. Its worsening is especially felt with efforts or during the night, making it impossible for the patient to sleep on the affected shoulder.
Also characteristic of shoulder bursitis is the presence of crackling that is palpable, or perceived by the patient, when mobilizing the joint, explains the orthopaedic doctor in Delhi.
Shoulder bursitis – causes
The most frequent causes of shoulder bursitis are trauma and repeated efforts, such as those that occur with certain work activities (painters or plasterers, warehouse replenishers, etc.) or with the practice of certain sports, such as weight training, swimming or others practiced with the arm above the head (“overhead sports”), says the sports injury specialist in west Delhi.
Certain rheumatic diseases (such as, for example, rheumatoid arthritis, gout, lupus, psoriatic arthritis) also often develop with bursitis (namely subacromial).
Shoulder bursitis – diagnosis
The diagnosis of this pathology is made, essentially, through a careful clinical examination, carried out by your specialist shoulder orthopaedic doctor in Delhi.
The exams to be performed later may be an x-ray that helps to exclude other causes of shoulder pain (such as osteoarthritis or calcifying tendinitis) and an ultrasound of the shoulder that easily visualizes the fluid in the subacromial bursa (caused by the inflammatory effusion).
The nuclear magnetic resonance (NMR) of the shoulder is, however, one that has a better diagnostic accuracy, obtaining high-resolution images of the surrounding muscle-tendon structures and eluding any intra-articular pathology, states the orthopaedic in West Delhi.
Is shoulder bursitis curable?
Shoulder bursitis is curable. Next, learn how to treat shoulder bursitis.
Shoulder bursitis – treatment
The medication or remedy most commonly used to treat shoulder bursitis is anti-inflammatory. The most common are ibuprofen, diclofenac, naproxen, among others. Its use is aimed at relieving pain and decreasing the inflammation that is always present in these conditions. Its application can be topical in the form of creams (or gels), or impregnated dressings that will make a prolonged release of these agents in the affected area.
The patient can also take these drugs in oral form (in capsules or diluted), taking care to do so after meals or preceded by taking gastric protectors, in order to avoid the aggression of the gastric or duodenal mucous membranes, states the orthopaedic doctor in Dwarka.
The physiotherapy is essential to maintain joint function and help control pain. A well-oriented physiotherapeutic treatment, with adequate exercises, can prevent the installation of a marked stiffness in the shoulder, usually called adhesive or retractable capsulitis (frozen shoulder or “frozen shoulder”). This would oblige to prolong the treatment for its complete resolution.
In cases of very acute and incapacitating pain, or reluctant to any other non-invasive treatment, infiltration or local injection of corticosteroids diluted with local anesthetic, may be a therapeutic weapon to be used by your orthopaedic doctor in Dwarka to resolve the condition. Your institution should be judicious and always consider the pros and risks of its application.
Shoulder bursitis – surgery
Shoulder arthroscopy in Delhi (surgery) is reserved for cases that are resistant to medical treatment or that simultaneously present other pathologies, such as rotator cuff tears or osteoarthritis, says the orthopaedic surgeon in Delhi.
This operation is performed using mini-invasive techniques that allow an excellent articular visualization, performing a minimal surgical aggression and thus providing a well-tolerated postoperative period and an easier and faster rehabilitation.
It should be carried out in specialized orthopaedic clinic in Delhi and by experienced orthopaedic surgeon in Delhi in order to obtain the best results.