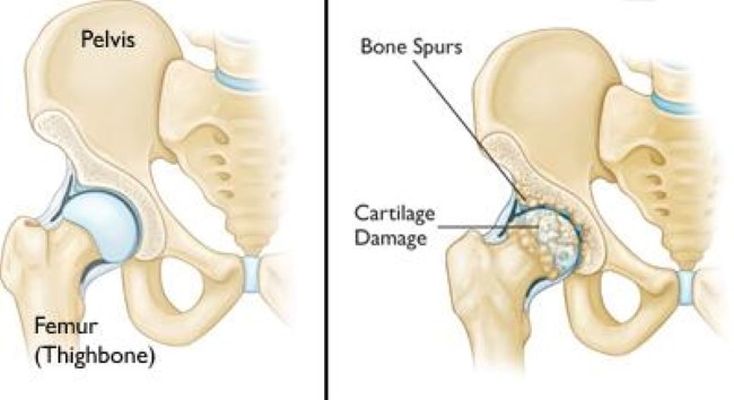
Coxarthrosis, or osteoarthritis of the hip joint, is a degenerative process characterized by the wear of the cartilage of the hip joint, as well as the formation of osteophytes and bone spikes along the perimeter of the joint. Clinically, coxarthrosis is manifested by contractures, stiffness in the hip joint, as well as atrophy of the muscles surrounding it. Coxarthrosis in the later stages leads to a significant decrease in the quality of life of the patient.
Initially, pain occurs after exercise, then the pain becomes constant and may even disturb sleep. Stiffness in the hip joint is first observed after a period of rest. Later, it progresses to such an extent that the patient has problems - for example, when putting on shoes or socks.
WHAT ARE THE CAUSES OF HIP ARTHROSIS?
When there is no clear cause for joint destruction, the term primary arthrosis is used in medicine.
Primary coxarthrosis is observed in 10-15% of people over 55 years of age. Women get sick more often than men. Osteoarthritis of the hip joint can occur without any apparent reason, but hard physical work and excessive physical activity can play a role in the development of the disease, for example, in sports, explains
orthopaedic in Delhi.
Secondary coxarthrosis occurs against the background of existing diseases and congenital malformations, such as hip dysplasia, systemic and metabolic bone diseases (for example, gout and pseudogout). These diseases lead to a change in the shape of the bones forming the hip joint, and also violate the structure and quality of the cartilage tissue.
In addition, diseases such as Perthes disease, HIV infection, injuries of the hip joint, aseptic necrosis and epiphysiolysis of the femoral head are predisposed to the formation of coxarthrosis.
Inflammatory diseases that subsequently lead to the development of coxarthrosis are rheumatoid arthritis, ankylosing spondylitis and systemic lupus erythematosus, says
orthopaedic in Dwarka.
SYMPTOMS OF COXARTHROSIS
Clinically, the disease is characterized by pain in the hip joint and lower limb, which initially occurs only at the beginning of the movement, but with the progression of the disease it is already present during movements, and at the final stage - even at rest. Pain is mainly localized in the groin, but can be reflected (radiating) to the knee. There is a decrease in the volume of all movements in the hip joint. In connection with the pain syndrome, lameness, joint stiffness, shortening of the limb appear and increase.
DIAGNOSIS OF COXARTHROSIS
In addition to the characteristic clinical picture, x-ray examination reveals a narrowing of the joint gap, bone spikes and osteophytes, deformation of the femoral head and acetabulum.
CONSERVATIVE TREATMENT
Pain and anti-inflammatory drugs can help the patient, and relief also brings warmth. Walking with a cane and physiotherapy exercises, aimed at maintaining mobility and stability in the hip joint, are recommended by
orthopaedic in West Delhi. In the early stages, manual therapy can permanently eliminate pain. In addition, it is desirable to reduce the load on the hip joint during daily activities.
SURGICAL TREATMENT
Indications for surgery are progressive intensification of pain, pain at night and at rest, a sharp limitation of the patient's functional capabilities and activity, as well as severe deformation and shortening of the leg.
In a typical case - a patient older than 40 years, with a long-term pain in the hip joint and increasing functional impairment - optimal operation is a
total hip replacement in Delhi. It reliably eliminates pain, restores mobility and ensures the stability of the hip joint.
WHEN CAN HIP REPLACEMENT REQUIRED?
The main indications for
hip replacement surgery in Delhi are arthrosis of the hip joint (coxarthrosis), fracture of the femoral neck, aseptic necrosis of the femoral head.
With arthrosis, degenerative changes in the articular cartilage occur, which ultimately leads to cartilage wear. Bone growths (osteophytes) form around the joint.
Due to the deterioration of the cartilage, a decrease in its thickness, a significant decrease in smoothness, as well as a change in the shape of the articular surfaces, the friction in the joint increases, which leads to pain and a progressive violation of the movements in the joint.
Aseptic necrosis of the femoral head is another cause of destruction of the hip joint. With this disease, the femoral head loses blood supply and actually collapses. The shape of the femoral head changes, the bone tissue making up the head is resorbed.
The articular surfaces of the acetabulum and the femoral head cease to correspond in shape, pain and impaired movement in the joint appear. The causes of the disease can be previous hip dislocations, birth injuries, prolonged treatment with corticosteroids, as well as some infections.
The main goal of replacing the joint in any of the degenerative diseases with an artificial one is to reduce pain and return movements. To do this, damaged surfaces are replaced with artificial ones, as a result of which the smoothness and painlessness of movements in the joint returns.
In case of fractures of the femoral neck, the blood supply to the head is disturbed, in connection with which its gradual destruction occurs.
Fracture fusion in these conditions is impossible, surgery is the only way to activate the patient and return him to everyday activity, says
orthopaedic surgeon in Delhi.